A non-invasive technology for correcting biomechanics
Meet Apos®
Introducing an innovative solution to help the body help itself relieve chronic knee,3,24 hip,28,29 or back26,27 pain effortlessly while wearing just 1 hour a day in the comfort of one’s home.
How Apos® is different
Apos® works on biomechanical and neuromuscular levels. Using a patented, foot-worn device as part of a daily treatment program, Apos® is designed to address the underlying causes of pain by temporarily shifting pressure from affected areas.
The neuromuscular re-education of the muscles results in a healthier walking pattern, even when not actively wearing the device.43
Apos® is clinically proven and FDA Cleared1 for knee OA
Over 40 peer-reviewed clinical studies document the positive impact of Apos®.
It’s not magic,
it’s science.
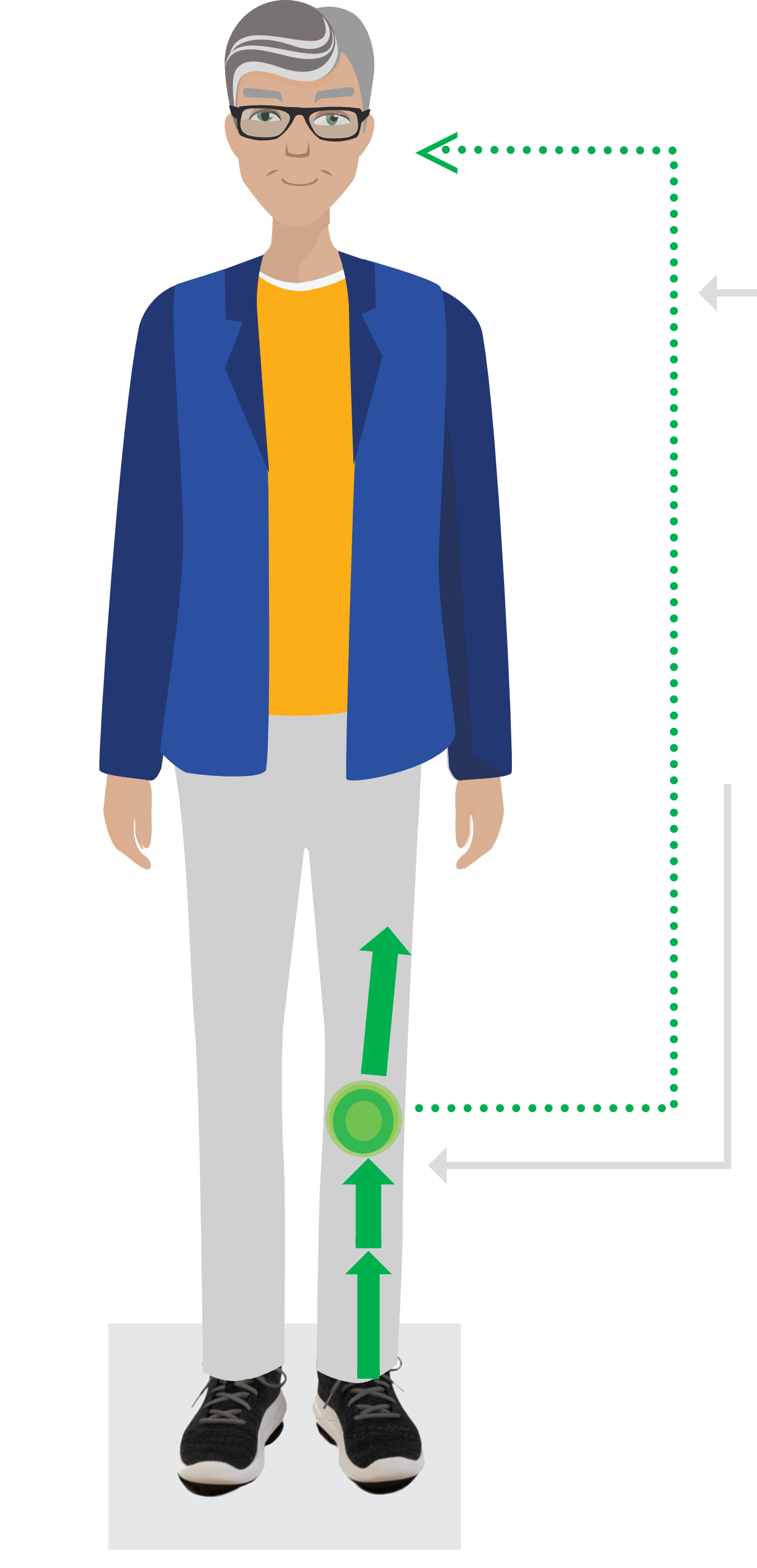
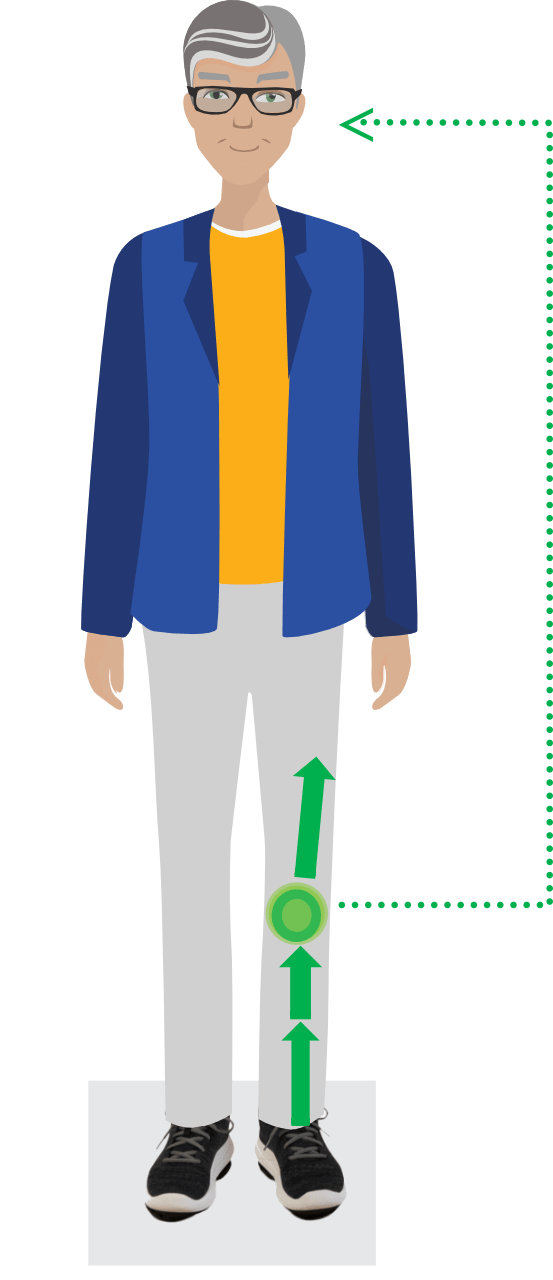
Neuromuscular retraining
The pods’ convexity creates micro-instability that increases proprioception and re-educates neuromuscular pathways43.
Biomechanical redistribution
Custom “pod” positioning changes the patient’s biomechanics, improves their gait, and directs forces away from unhealthy joint compartments7.
Initial Assessment
Computerized gait test
The Apos® device is customized and calibrated at the initial assessment.
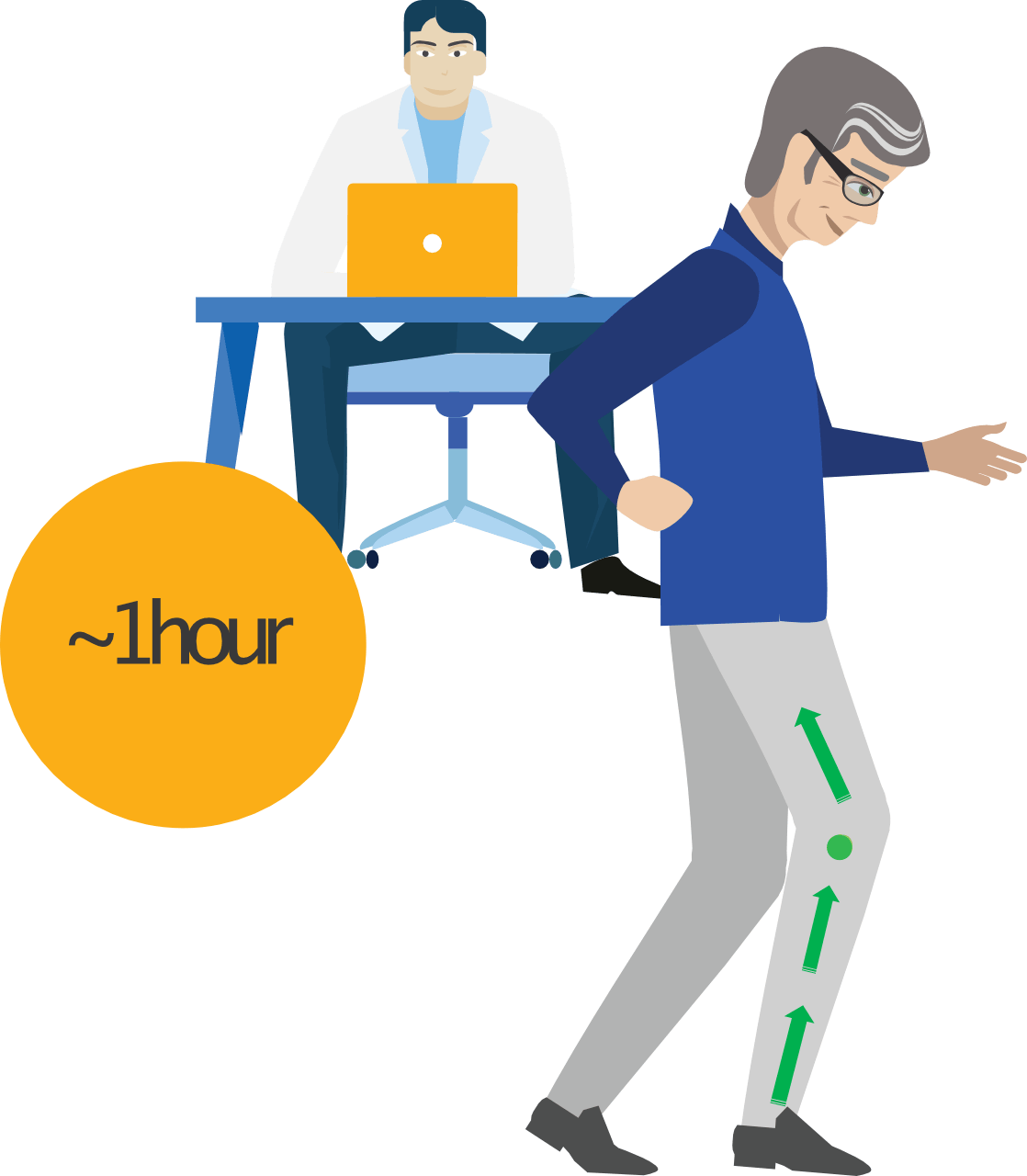
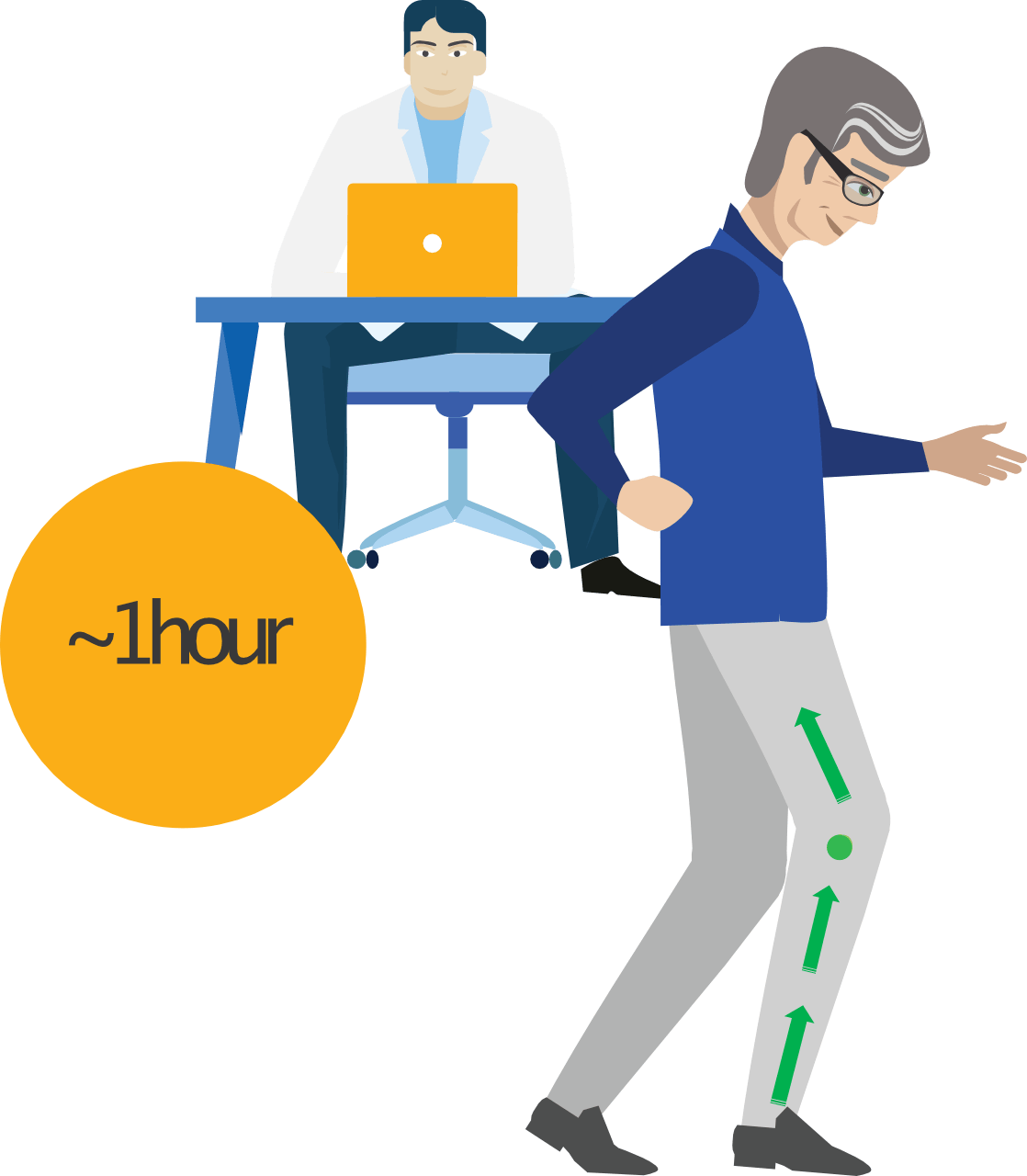
Treatment
Passive home treatment
Simply wearing the device for about an hour daily around the home re-educates gait.43
Recalibration visits
Increased ‘pod’ convexity every few months challenges the patient’s muscles to improve in stability45 and coordination.43
Live Again
Getting back to life
The neuromuscular training leads to lasting pain relief43 and improved function43 even when not wearing the device.43
Initial Assessment
Treatment
Live Again
Computerized gait test
The Apos® device is customized and calibrated at the initial assessment.
Passive home treatment
Simply wearing the device for about an hour daily around the home re-educates gait.43
Recalibration visits
Increased ‘pod’ convexity every few months challenges the patient’s muscles to improve in stability45 and coordination.43
Getting back to life
The neuromuscular training leads to lasting pain relief43 and improved function43 even when not wearing the device.43
Getting your clinicians to be an Apos® Trained Professional (ATP) is now easier than ever.
Clinicians who successfully complete this course will be recognized as an Apos® Trained Professional (ATP). A resume booster for your clinicians!
1 Day Training
In Classroom

Up To 2 Days Of Real Patient Hands-On Experience

Start using Apos® for your patients
Complete the form below to be contacted by our Apos® business development team.

